Resistance major obstacle in malaria control
The therapeutic options for malaria are scarce and massively challenged by the emergence of resistant parasite strains, which causes a major obstacle to malaria control.
To prevent a potential public health emergency, there is an urgent need for new antimalarial drugs, with single-dose cures, broad therapeutic potential, and novel mechanism of action. Antimalarial drug development can follow several approaches ranging from modifications of existing agents to the design of novel agents that act against novel targets. Modern advancement in the biology of the parasite and the availability of the different genomic techniques provide a wide range of novel targets in the development of new therapy. Several promising targets for drug intervention have been revealed in recent years. Therefore, this review focuses on the progress made on the latest scientific and technological advances in the discovery and development of novel antimalarial agents. Among the most interesting antimalarial target proteins currently studied are proteases, protein kinases, Plasmodium sugar transporter inhibitor, aquaporin-3 inhibitor, choline transport inhibitor, dihydroorotate dehydrogenase inhibitor, isoprenoid biosynthesis inhibitor, farnesyltransferase inhibitor and enzymes are involved in lipid metabolism and DNA replication. This review summarizes the novel molecular targets and their inhibitors for antimalarial drug development approaches.
Background
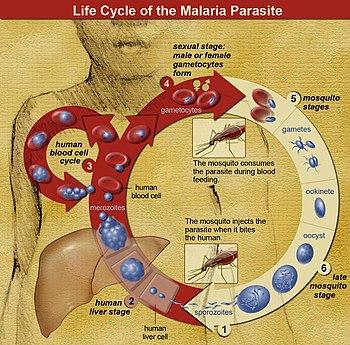
Malaria is a devastating parasitic infectious disease, especially in Sub-Saharan African, parts of Asia, and South America. Even though several efforts undertaken, nowadays, it is one of the major causes of morbidity and mortality, mainly in pregnant women and children. The five identified Plasmodium species responsible for inflicting malaria in humans are P. vivax, P. knowlesi, P. ovale, P. malariae, and P. falciparum. Of these, P. falciparum is the most virulent and prevalent Plasmodium species.
In the absence of an effective vaccine, the therapeutic use of antimalarial agents remains the only method for management and prophylaxis of malarial disease. Several studies showed that the efficacies of most antimalarial agents compromised by the emergency of drug-resistant Plasmodium species.
Resistance reported for nearly all available antimalarial agents that reinforced the urgent need to develop new antimalarial agents against existing validated targets, as well as to search for novel targets.
The development of a novel antimalarial agent that acts toward both transmissible gametocytes stages and the intraerythrocytic proliferative asexual, in particular, those of resistant parasite species, is urgently required. Several enzymes, ion channels, transporters, interacting molecules in red blood cell (RBC) invasion, and molecules responsible for oxidative stress in the parasite, lipid metabolism, and degradation of hemoglobin are promising novel targets to develop new antimalarial drugs against rapidly mutating malarial parasites.7
The new antimalarial agent should have the efficacy to prevent infection (chemoprotective agents), and clear P. vivax hypnozoites from the liver (anti-relapse agents).
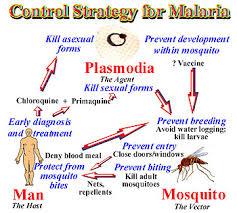
Traditional drug discovery follows many approaches to identifying a new ant-malarial agent to combat malaria disease. These approaches are optimization of current drug regimens and formulations, modifying the existing antimalarial agents, screening of natural products, isolating resistance-reversal agents, utilizing combination chemotherapeutic approaches, and exploiting drugs indicated for other uses.
Besides the traditional drug discovery methods for the identification of new ant-malarial agent, the understanding of Plasmodium cell biology and genome has proved a powerful tool for uncovering mechanisms of resistance, and have great potential to design a novel drugs with both high antimalarial activity and transmission-blocking potential to combat malaria once and for all.
The new drug should: (i) address drug-resistance issues, (ii) have a rapid onset of action, (iii) be safe, especially in children and pregnant women, and (iv) cure malaria in a single dose. The challenge is to find a drug that addresses all of these features.
Currently, most antimalarial agents are targeting the asexual phase of malaria infection that causes symptomatic illness. The existing antimalarial agents grouped into three main classes: quinoline derivative, antifolate, and artemisinin derivatives. There is no single drug that has been identified or manufactured that can wipe out all strains of the Plasmodium species. Thus, to fight malarial infection efficiently, a combination of drugs is frequently administered at the same time. Quinolines are the most widely used antimalarial agents for the management of malaria. Quinine is an alkaloid isolated from the bark of Cinchona trees, was the first antimalarial agent used for the management of disease in the 17th century. Quinine became the standard therapy for malaria from the mid-19th century to the 1940s. The emergence of resistant strains of P. falciparum, in addition to toxicity, has limited the therapeutic use of Quinine. However, Quinine is still used against severe malaria, most often combined with a second agent to decrease treatment duration and to minimize the side effects.
Chloroquine was developed during World War II to treat malaria. Chloroquine is a drug of choice to treat malarial due to its efficacy, safety, and low cost, however its irrational use soon led to the emergence of chloroquine-resistant P. falciparum species.
Sources: dovepress.com; malariasite.com; who.com
Background
Malaria is a devastating parasitic infectious disease, especially in Sub-Saharan African, parts of Asia, and South America. Even though several efforts undertaken, nowadays, it is one of the major causes of morbidity and mortality, mainly in pregnant women and children. The five identified Plasmodium species responsible for inflicting malaria in humans are P. vivax, P. knowlesi, P. ovale, P. malariae, and P. falciparum. Of these, P. falciparum is the most virulent and prevalent Plasmodium species.
In the absence of an effective vaccine, the therapeutic use of antimalarial agents remains the only method for management and prophylaxis of malarial disease. Several studies showed that the efficacies of most antimalarial agents compromised by the emergency of drug-resistant Plasmodium species.
Resistance reported for nearly all available antimalarial agents that reinforced the urgent need to develop new antimalarial agents against existing validated targets, as well as to search for novel targets.
The development of a novel antimalarial agent that acts toward both transmissible gametocytes stages and the intraerythrocytic proliferative asexual, in particular, those of resistant parasite species, is urgently required. Several enzymes, ion channels, transporters, interacting molecules in red blood cell (RBC) invasion, and molecules responsible for oxidative stress in the parasite, lipid metabolism, and degradation of hemoglobin are promising novel targets to develop new antimalarial drugs against rapidly mutating malarial parasites.7
The new antimalarial agent should have the efficacy to prevent infection (chemoprotective agents), and clear P. vivax hypnozoites from the liver (anti-relapse agents).
Traditional drug discovery follows many approaches to identifying a new ant-malarial agent to combat malaria disease. These approaches are optimization of current drug regimens and formulations, modifying the existing antimalarial agents, screening of natural products, isolating resistance-reversal agents, utilizing combination chemotherapeutic approaches, and exploiting drugs indicated for other uses.
Besides the traditional drug discovery methods for the identification of new ant-malarial agent, the understanding of Plasmodium cell biology and genome has proved a powerful tool for uncovering mechanisms of resistance, and have great potential to design a novel drugs with both high antimalarial activity and transmission-blocking potential to combat malaria once and for all.
The new drug should: (i) address drug-resistance issues, (ii) have a rapid onset of action, (iii) be safe, especially in children and pregnant women, and (iv) cure malaria in a single dose. The challenge is to find a drug that addresses all of these features.
Currently, most antimalarial agents are targeting the asexual phase of malaria infection that causes symptomatic illness. The existing antimalarial agents grouped into three main classes: quinoline derivative, antifolate, and artemisinin derivatives. There is no single drug that has been identified or manufactured that can wipe out all strains of the Plasmodium species. Thus, to fight malarial infection efficiently, a combination of drugs is frequently administered at the same time. Quinolines are the most widely used antimalarial agents for the management of malaria. Quinine is an alkaloid isolated from the bark of Cinchona trees, was the first antimalarial agent used for the management of disease in the 17th century. Quinine became the standard therapy for malaria from the mid-19th century to the 1940s. The emergence of resistant strains of P. falciparum, in addition to toxicity, has limited the therapeutic use of Quinine. However, Quinine is still used against severe malaria, most often combined with a second agent to decrease treatment duration and to minimize the side effects.
Chloroquine was developed during World War II to treat malaria. Chloroquine is a drug of choice to treat malarial due to its efficacy, safety, and low cost, however its irrational use soon led to the emergence of chloroquine-resistant P. falciparum species.
Sources: dovepress.com; malariasite.com; who.com





Kommentaar
Republikein
Geen kommentaar is op hierdie artikel gelaat nie